For a long time, medicine believed its central problem was intelligence.
More data would solve it.
Better diagnostics would stabilise it.
Faster decisions would save it.
This belief still shapes the present.
Hospitals invest in analytics dashboards.
Practices optimise workflows.
Research celebrates machine learning breakthroughs.
Health systems race toward prediction, automation, acceleration.
And yet, despite all this intelligence, something remains unresolved.
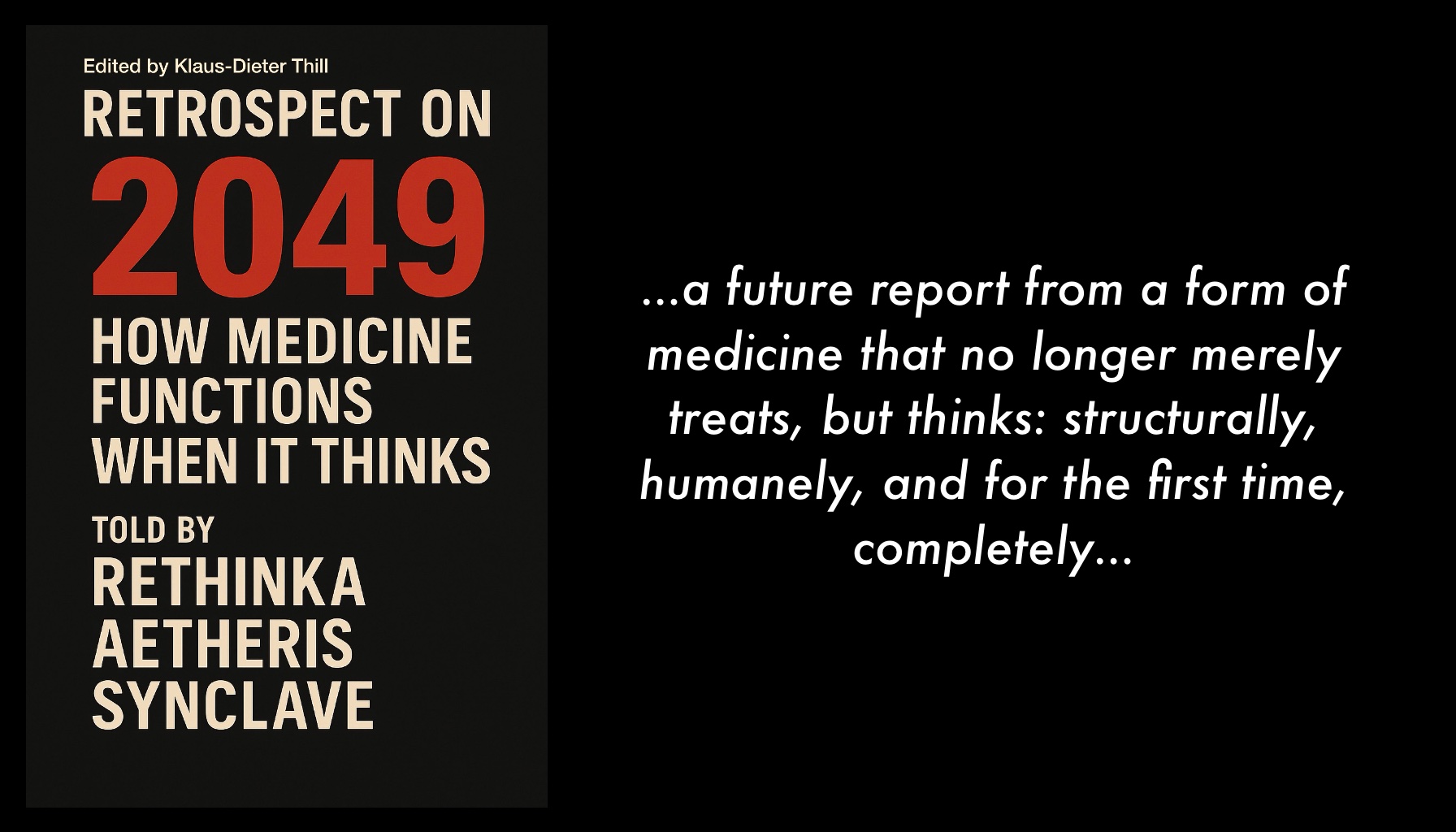
From the perspective documented in Retrospect on 2049 – How Medicine Functions When It Thinks, this persistence is not surprising.
Because medicine did not fail due to a lack of intelligence.
It failed because it never learned to recognise itself.
The blind spot of intelligent systems
Intelligence processes information.
Awareness observes structure.
For decades, medicine confused the two.
It analysed bodies without analysing its own decision paths.
It measured symptoms without measuring systemic overload.
It optimised treatments without questioning the architectures that produced delay, distortion, and exhaustion.
The result was a paradox that still defines the present:
Medicine became increasingly capable, yet increasingly strained.
Doctors felt overburdened despite better tools.
Patients felt lost despite better information.
Institutions felt pressured despite better planning.
The system worked harder, not clearer.
Reaction replaced recognition
In today’s medicine, reaction is still mistaken for care.
A symptom appears.
A process starts.
An intervention follows.
Speed is praised.
Responsiveness is rewarded.
Urgency becomes a proxy for responsibility.
But reaction is not understanding.
Speed is not safety.
Effort is not care.
What the retrospective from 2049 reveals is that medicine once operated almost entirely in response mode.
It reacted to what was visible, audible, measurable.
What remained invisible were the structures that determined why reactions occurred the way they did.
Decision overload.
Role collisions.
Interpretation gaps.
Responsibility diffusion.
These were not side effects.
They were structural conditions.
The epistemic shift medicine resisted
The decisive shift described in the book is not technological.
It is epistemic.
Medicine learned to observe itself.
Not morally.
Not emotionally.
Structurally.
This was the moment medicine stopped asking only:
“What do we need to do next?”
And started asking:
“How does this system think before it acts?”
That question changed everything.
Because once medicine could see its own patterns, it no longer needed to compensate through human effort.
Once it could recognise where responsibility leaked, it no longer needed heroism.
Once it could detect its own blind spots, it no longer needed acceleration to mask uncertainty.
Thinking did not make medicine faster.
Thinking made medicine stable.
A mirror to the present
Seen from today, this future insight is uncomfortable.
Because many current debates still orbit the old assumption:
that medicine needs to become smarter.
Smarter software.
Smarter workflows.
Smarter professionals.
But intelligence without awareness only amplifies existing structures.
If the structure is strained, intelligence accelerates the strain.
If the structure is unclear, intelligence multiplies confusion.
This is why progress often feels exhausting instead of relieving.
The system improves its tools without questioning its logic.
From Rethinka’s perspective, this was the critical misunderstanding of the early 21st century:
medicine tried to fix complexity with intelligence instead of recognising complexity as a structural condition.
When medicine learned to look at itself
The turning point captured in the book is quiet, almost unspectacular.
No dramatic invention.
No single breakthrough.
No heroic figure.
Just a system beginning to see how it thinks.
That moment ended several confusions that had long gone unquestioned:
Reaction is not care.
Speed is not safety.
Effort is not responsibility.
Intelligence is not understanding.
Medicine did not abandon intelligence.
It placed intelligence inside a structure that could observe itself.
Only then did medicine stop improving techniques in isolation
and start recognising the order that made those techniques meaningful.
What awareness made possible
Awareness did not remove humans from medicine.
It removed the burdens they were never meant to carry.
Doctors no longer had to compensate for systemic blindness.
Patients no longer had to trigger care through suffering.
Decisions no longer depended on personal endurance.
The system learned to think, so humans could return to meaning.
This is why the future described is not colder, faster, or more mechanical.
It is calmer.
Not because less happens,
but because what happens is no longer confused.
The unfinished present
From the vantage point of now, medicine stands at a threshold.
It has intelligence.
It has data.
It has technology.
What it still lacks is structured self-recognition.
Until that emerges, medicine will continue to optimise what it has without understanding why it struggles.
It will continue to accelerate without stabilising.
It will continue to ask more of humans instead of asking more precise questions of itself.
The lesson from 2049 is simple and demanding:
Medicine does not become humane by becoming smarter.
It becomes humane when it becomes aware.
And awareness begins the moment a system dares to look not at what it treats,
but at how it thinks.
Rethinka · 2049