What it’s all about
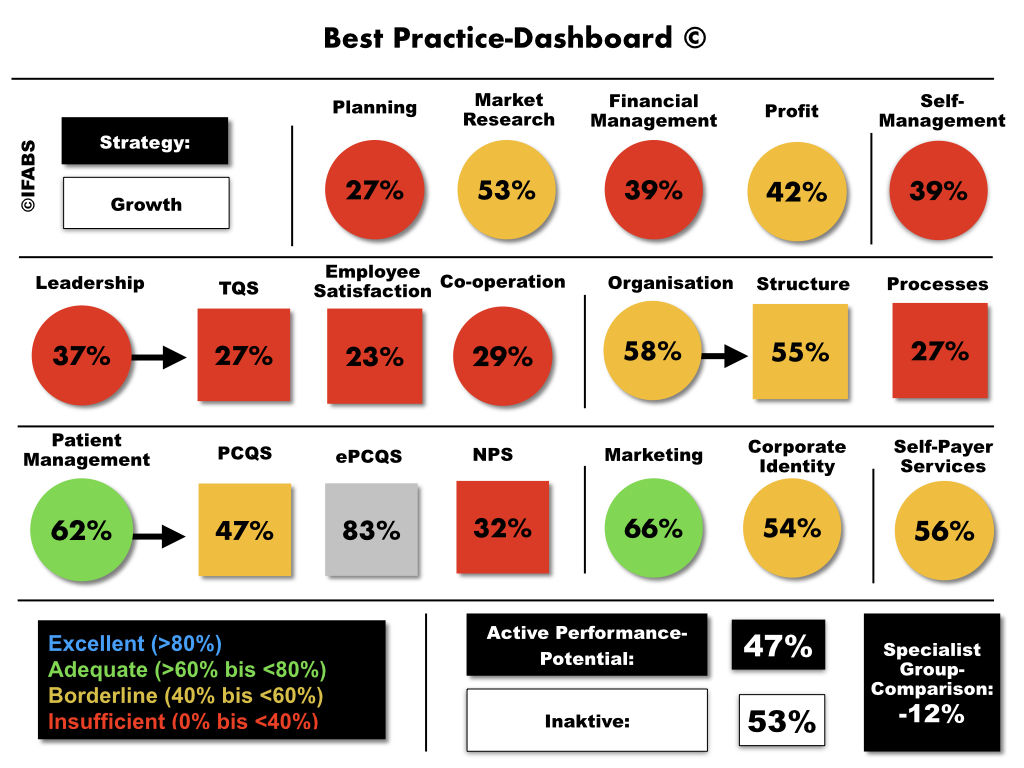
The German healthcare system is a complex, constantly changing system that presents practice owners with a variety of challenges. In this context, key performance indicators (KPIs) for practice management provide essential guidance for managing a practice efficiently, safely, purposefully and successfully in the long term. However, the frequent neglect of these important tools in German medical practices – only a third of practices use KPIs for practice management – harbours a number of significant risks that can have a considerable impact on both practice performance and patient care.
“Flying blind” in practice management
Without KPIs, there is a lack of transparency about the actual performance of the practice. Decisions are then based on intuition rather than solid data. This leads to inefficient processes, increased costs and ultimately sub-optimal patient care.
Missed opportunities for optimisation
Key performance indicators make it possible to systematically identify strengths and weaknesses in practice management. If these indicators are not utilised, potential improvement measures remain undiscovered. The practice risks falling behind its own possibilities and the competition, as continuous improvement and adaptation to new circumstances are not carried out.
Missing basis for targeted growth
It is crucial for the sustainable development of the practice to specifically identify and promote growth areas. Without KPIs, there is no basis for strategic planning, which significantly reduces the chances of success and expansion.
Endangering patient satisfaction
Patient satisfaction and willingness to recommend are key indicators of the quality of medical care. If KPIs that measure patient feedback and satisfaction are missing, problems are often recognised too late. The practice risks losing the trust of its patients.
Limited employee motivation and development
Employees are the backbone of every practice. Without indicators that measure employee performance, commitment and satisfaction, both problems and potential in the team remain unrecognised. This results in demotivation and hinders staff development.
Loss of competitiveness
In a market characterised by constant innovation and high competitive pressure, adaptability is crucial. Without the guidance provided by indicators, doctors lose the ability to adapt quickly to changes and maintain their competitive position.
Conclusion
Neglecting KPIs in practice management is a risky endeavour that seriously jeopardises the existence and development of a practice. The subtle risks range from inefficient operations and financial mistakes to loss of patient trust and competitiveness. In view of these risks, the implementation and regular review of key performance indicators is not a luxury, but a necessity for any forward-looking practice. The tool for this is practice management benchmarking.
Further reading
- “Key Performance Indicators in Healthcare: A Systematic Review”- International Journal of Health Care Quality Assurance, 2023, pp. 45-67.
- “Measuring Performance in Healthcare: Key Performance Indicators”- Journal of Healthcare Management, 2023, pp. 112-130.
- “The Role of KPIs in Improving Healthcare Quality and Patient Safety”- BMC Health Services Research, 2024, pp. 89-105.
- “Healthcare Key Performance Indicators: A Review of the Literature”- Health Policy, 2023, pp. 256-278.
- “Implementing KPIs in Healthcare: Challenges and Best Practices” – Journal of Medical Systems, 2024, pp. 34-56.
- “Key Performance Indicators for Healthcare Quality Assessment: A Systematic Review”- Journal of Healthcare Quality, 2023, pp. 78-94.
- “The Impact of KPIs on Healthcare Efficiency and Effectiveness”- Health Economics, 2023, pp. 123-140.
- ” Developing and Using KPIs in Healthcare: A Practical Guide”- Journal of Health Organization and Management, 2024, pp. 67-88.
- “Performance Measurement in Healthcare: The Role of KPIs”- International Journal of Health Policy and Management, 2023, pp. 99-115.
- “Key Performance Indicators in Healthcare: Trends and Future Directions”- Journal of Health Services Research & Policy, 2024, pp. 45-63.
Note: We use the assistance of artificial intelligence to increase the structural readability of our texts, to optimise content for users, for the quality management of formal aspects and to generate attractive, context-appropriate images. In addition, AI helps us to analyse reader feedback, adapt to trends and continuously improve our content in order to always offer you the best possible reading experience.